A Revitalized Community Medicine Course for Third-Year Medical Students
Leslie Patterson, PhD, and Rebecca Bernstein, MD, Department of Family and Community Medicine, Medical College of Wisconsin
Health disparities are of great concern nationally and in the urban neighborhoods near our medical school (Milwaukee, WI).1 A high-quality community medicine experience is of critical importance to prepare medical students to care for underserved populations. The Department of Family and Community Medicine at the Medical College of Wisconsin (MCW) has included a community medicine course as a longstanding component of the M3 Family Medicine Clerkship. The community medicine curriculum seeks to help students develop an understanding of the sociocultural, economic, and environmental factors that influence a patient's health and to understand the role of the family physician in incorporating these issues into an appropriate plan of care.
MCW’s M3 Family Medicine Clerkship is a 4-week required rotation where medical students spend 1 day per week participating in team-based learning sessions (TBL); the rest of the week is spent in clinic. There are four main components of the community medicine course: (1) Orientation to Community Medicine Concepts, (2) Participation in the Community Medicine TBL session, (3) Completion of a community-based experience (eg, home visit, volunteer at un/under-insured clinic, community health education presentation, in-depth patient interview on social history), and (4) Completion of a reflection paper. The orientation is a 30-minute session that occurs on the first day of the rotation and introduces students to the ways in which socioeconomic status, culture, and health literacy impact health and health-seeking behaviors. The TBL session is a 4-hour session that occurs during the third week. In preparation for the TBL session, students read selected chapters from two books and two peer-reviewed articles that focus on health disparities and social determinants of health.2-5 Students complete a six question multiple choice quiz at the start of the TBL session to evaluate their comprehension of the readings. The quiz counts for 2% of their final clerkship grade. Additional topics covered in the TBL session include empathy, implicit bias, and access to community assets and resources to address patient needs. Students complete their community-based experiences throughout the 4 weeks; each experience requires 1 half day. The reflection papers are based on the students’ community-based experiences. Course instructors grade the papers using a rubric that assesses the students’ ability to identify and describe socioeconomic, cultural, and health education issues impacting the patient/clients’ health and how they addressed the issue during the experience. The reflection paper represents 10% of the students’ final clerkship grade.
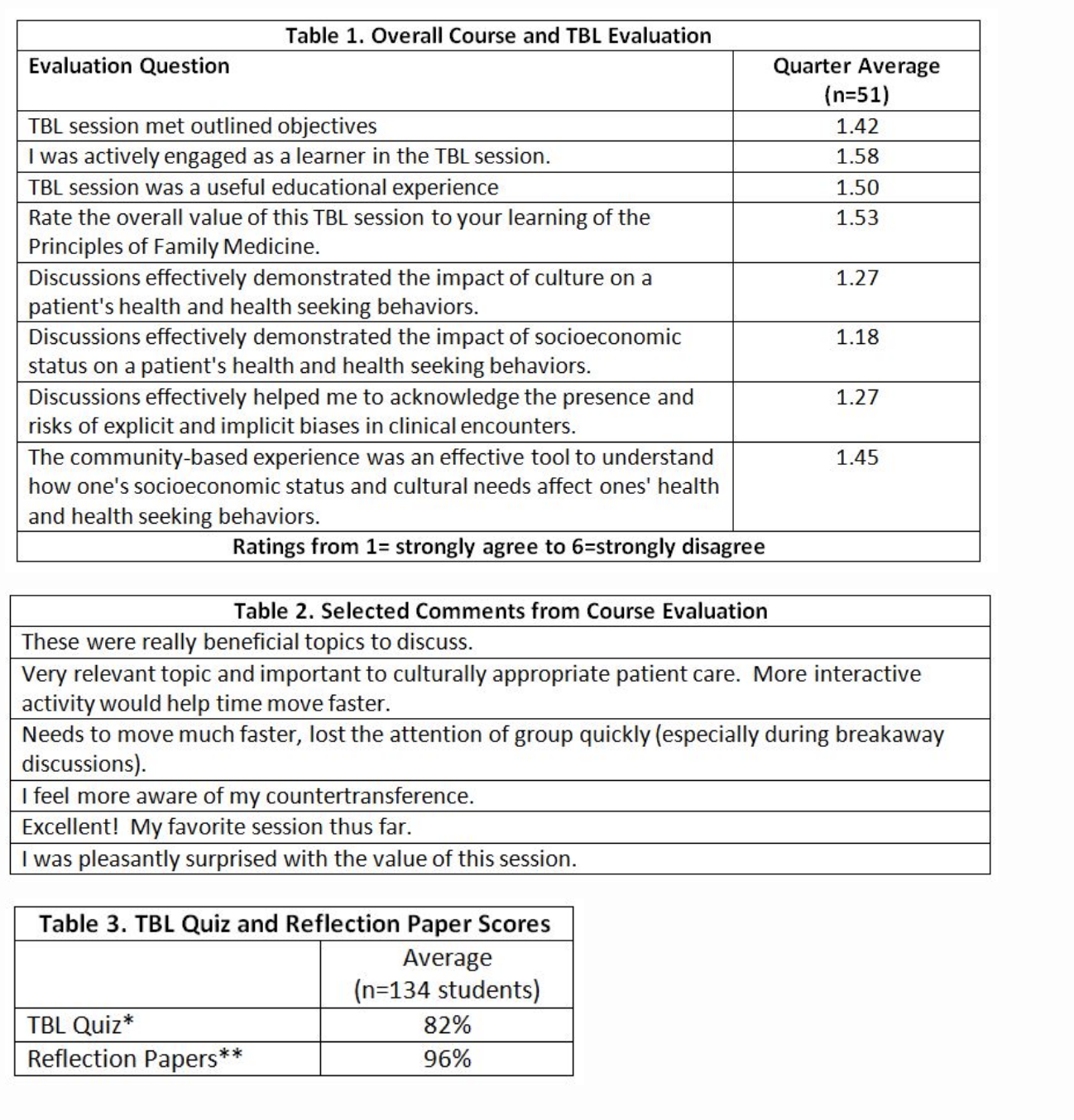
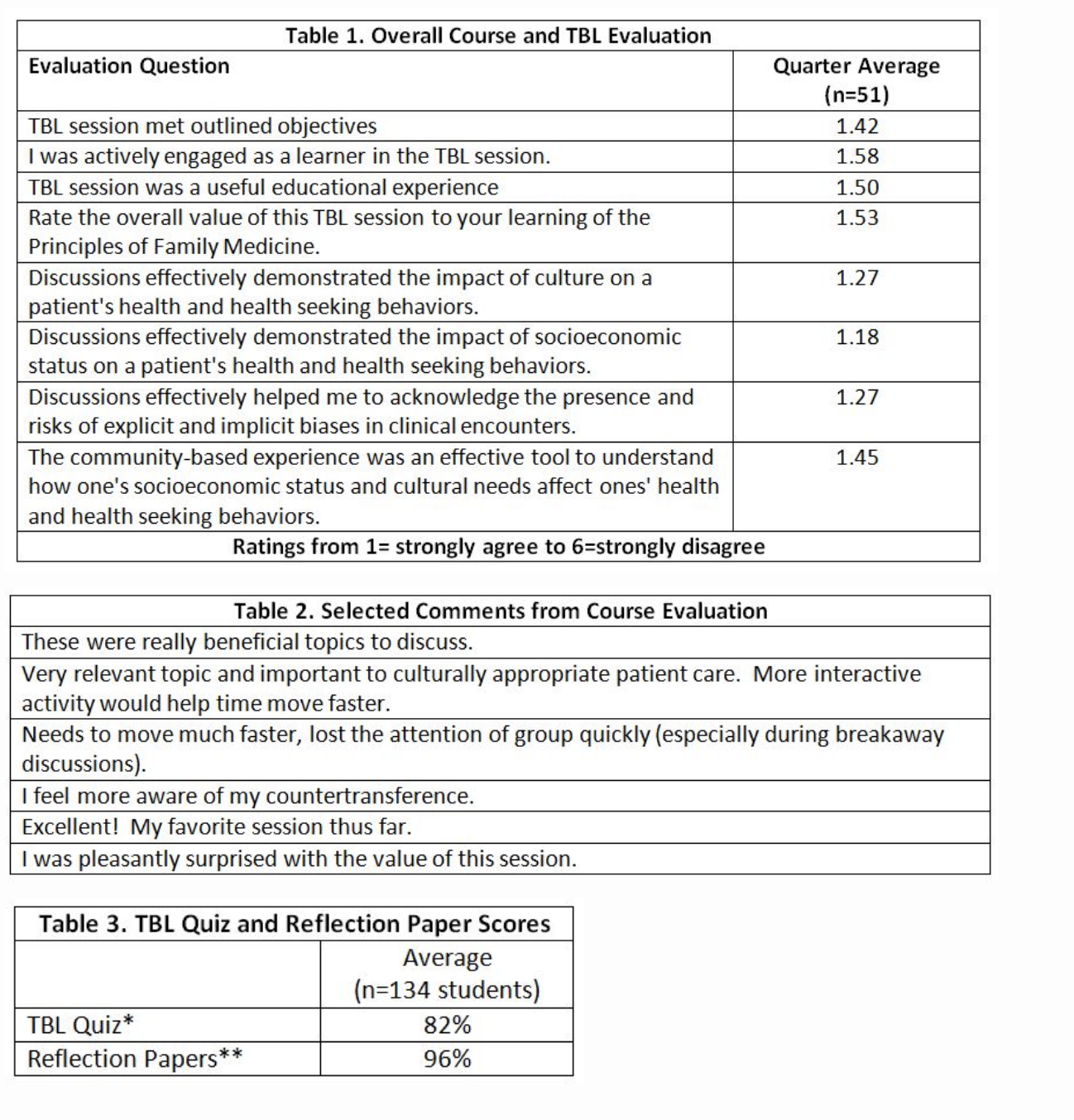
We evaluated the community medicine course using Kirkpatrick’s Model of training evaluation, focusing on outcomes at Levels 1–3 (Reaction, Learning, Behavior Change).6 To assess Reaction outcomes, students complete session evaluations on paper forms after the community medicine TBL session. This data, both quantitative scores and qualitative student comments, are entered electronically by department staff and summarized quarterly. Reaction data for the most recent quarter was favorable (Tables 1 and 2). To capture outcomes related to Learning and Behavior Change, we reviewed scores on TBL quizzes and reflection papers from the first 8 months of the current academic year (Table 3).
The community medicine course taught as part of the M3 Family Medicine Clerkship assists students in incorporating knowledge of societal issues and community resources into their clinical exam skills. The course, mainly its evaluation, is limited by challenges associated with assessing the degree to which students are fully engaged with implementing course concepts (ie, Behavior Change) and the course’s true impact on influencing students’ future practice of medicine. Despite this challenge, we conclude that including a community medicine course (in the Family Medicine Clerkship) can positively impact students’ views about family medicine.
For questions regarding the community medicine course, email Leslie Patterson, PhD (lpatterson@mcw.edu).
References
- IOM Report: Unequal Treatment: Confronting racial and ethnic disparities in healthcare. Washington, DC: Institute of Medicine, 2003.
- Fadiman A. The spirit catches you and you fall down. New York: Farrar, Straus and Giroux, 1997.
- Manheimer E. Twelve patients: life and death at Bellevue Hospital. New York: Grand Central Publishing, 2012.
- Lantz PM, Golberstein E, House JS, Morenoff D. Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of US adults. Soc Sci Med 2010;70:1558-66.
- Carrillo JE, Green AR, Betancourt JR. Cross-cultural primary care: a patient-based approach. Ann Intern Med 1999;130:829-34.
- Kirkpatrick D, Kirkpatrick J. Evaluating training programs: the four levels, third edition. San Francisco: Berrett Koehler, 2006.
*Additional references available from author upon request