Improving Diagnosis of Migraine in Primary Care
Karly Pippitt, MD
Headache is a common complaint in primary care, and migraines affect approximately 12% of the US population;1 however, most medical schools offer only about 3 hours of education on headache.2,3 This distinction between headache and migraine is important, as correct diagnosis makes correct treatment more likely.
In our review of patients in our community clinics, we found the predominant diagnosis was of headache, not migraine, and the corresponding prescription for this diagnosis was an opiate pain medication, which is known to make migraine headaches worse.4
There are many possible approaches to addressing an educational gap such as this one. We decided to use a validated screening tool, ID Migraine,5 embedded into the electronic medical record with the goal of increasing diagnosis rates of migraine while decreasing rates of the diagnosis of a nonspecific headache. The ID MigraineTM tool consists of three short questions:
- In the last 3 months, did you feel nauseated or sick with a headache?
- In the last 3 months, did light bother you with a headache?
- In the last 3 months, have your headaches limited your ability to work, study, or do your daily activities for at least a day?
Answering “yes” to two out of three questions yields > 80% probability of a diagnosis of migraine. The intervention was administration of this questionnaire by the medical assistant when checking in patients over a 6-week period in our two residency clinics.
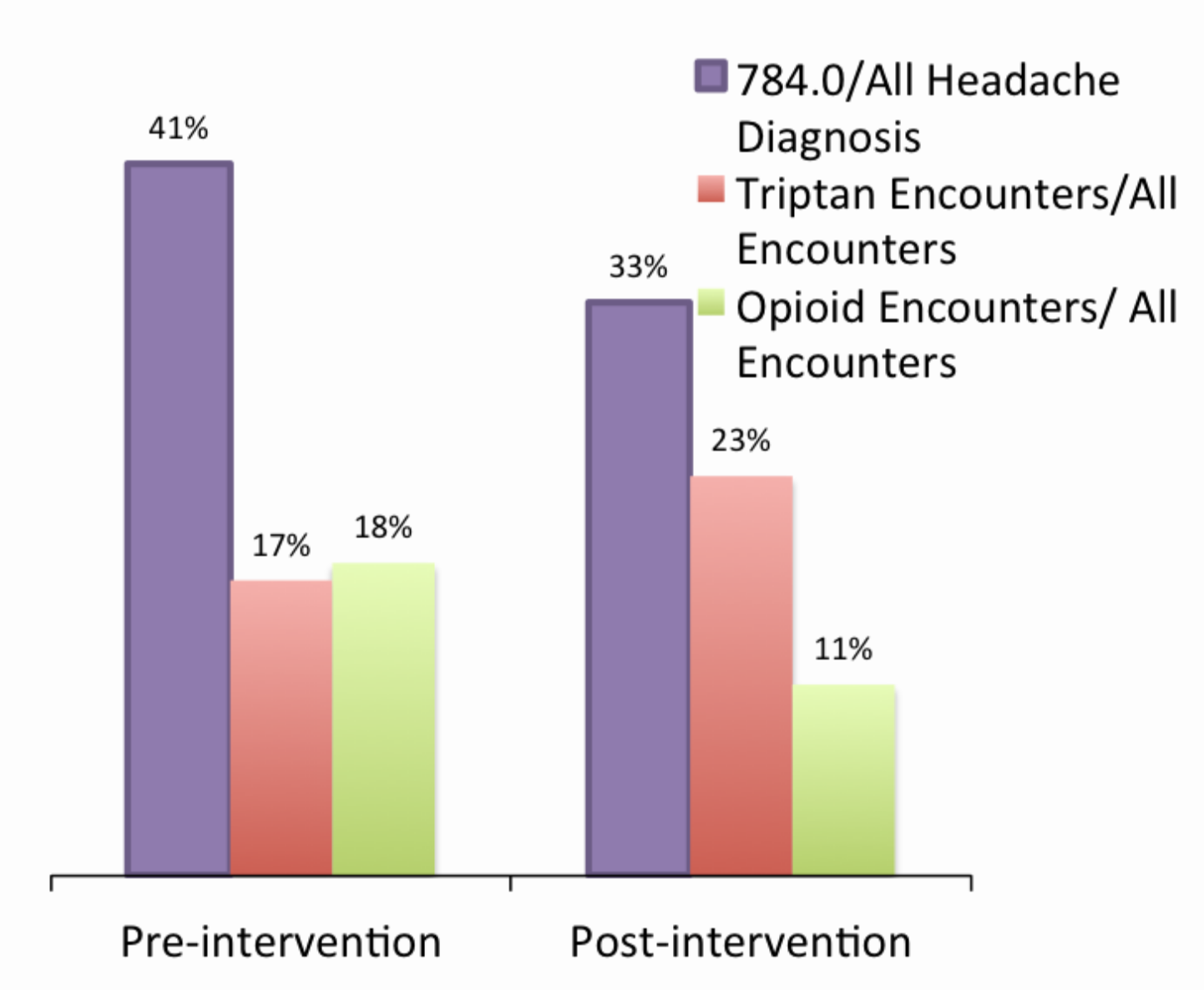

In this short time, a 20% relative reduction in diagnosis of “headache” was seen, there was a 36% increase in use of triptan medications, and a 37% reduction in associated opioid prescription use with headache. This questionnaire is currently being extended to all of our community clinics. The results might be more dramatic system wide because our residency clinics had the lowest numbers of headache diagnosis and associated opioid use. While the ID MigraineTM is intended to help diagnose migraine, it is reasonable to use this in follow-up visits for migraine headaches, since most patients suffering from migraines will still have a positive screen, this helps ensure the correct diagnosis and treatment.
There has been some push back in utilization from physicians, particularly from those who feel comfortable with the accurate diagnosis of migraine. Utilization has been high with new trainees, likely due to increased confidence in diagnosis. By having the medical assistant take this information on intake, this information is then available to the clinician. If this is not done on intake, these questions are typically answered while taking the history; the tool is there to help providers be aware of the significance of these historical elements.
A major part of the success of tool usage was getting this embedded into the electronic medical record. As this project was rolled out as part of the LEAN program, there was IT support given to each group. This has the potential to be a major hurdle for clinics using an EMR without the ability or support to make changes to the EMR, though these three questions could easily be included into an intake form for patients.
References
- Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 2001 Jul-Aug;41(7):646-57.
- Finkel AG. American academic headache specialists in neurology: practice characteristics and culture. Cephalalgia: an international journal of headache 2004 Jul;24(7):522-7.
- Gallagher RM, Alam R, Shah S, Mueller L, Rogers JJ. Headache in medical education: medical schools, neurology and family practice residencies. Headache 2005 Jul-Aug;45(7):866-73.
- Mattson DH, Lisak RP, Jones DE, et al. The American Academy of Neurology's top five Choosing Wisely recommendations. Neurology 2013 Sep;81(11):1022-3.
- Lipton RB, Dodick D, Sadovsky R, et al. A self-administered screener for migraine in primary care: The ID Migraine Validation Study. Neurology 2003 Aug 12;61(3):375-82.