The Peer Instruction Method: An Alternative Approach for Facilitating Interprofessional Education
John Bucheit, PharmD, BCACP, CDE, Mercer University College of Pharmacy; Ruchi Patel, MD; Robert Pallay, MD, Memorial Family Medicine Residency Program, Mercer University
The evolving landscape of health care necessitates a change in education and training for future health care professionals. New models, including patient-centered medical homes and Accountable Care Organizations, highlight the need for team-based care to optimize patient outcomes. Many medical and pharmacy schools are providing joint education in response to these changes. This challenging task is consistent with the Interprofessional Education Collaborative (IPEC), which provides guidance for interprofessional education (IPE).1 According to IPEC, a better understanding of the following core competencies should be incorporated into IPE learning: values/ethics, roles/responsibilities, communication, and teamwork.1 Eager to expose medical and pharmacy trainees to IPE, Memorial Family Residency Program developed a training session using the Peer Instruction Method.
The Peer Instruction Method
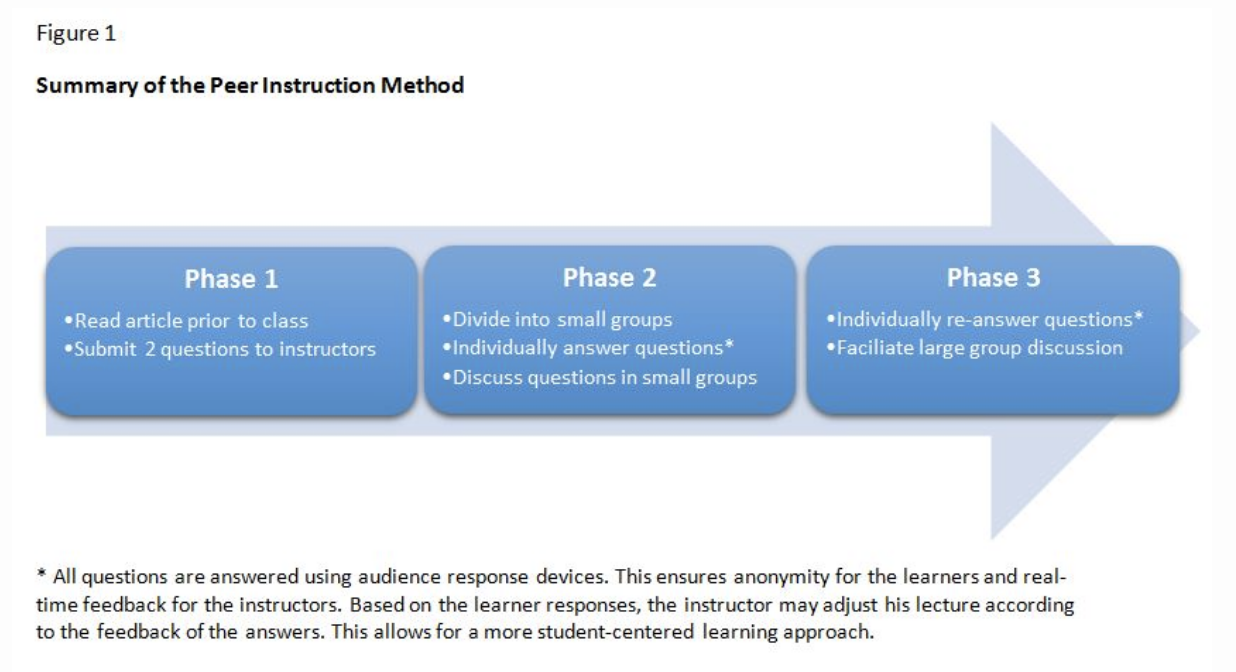
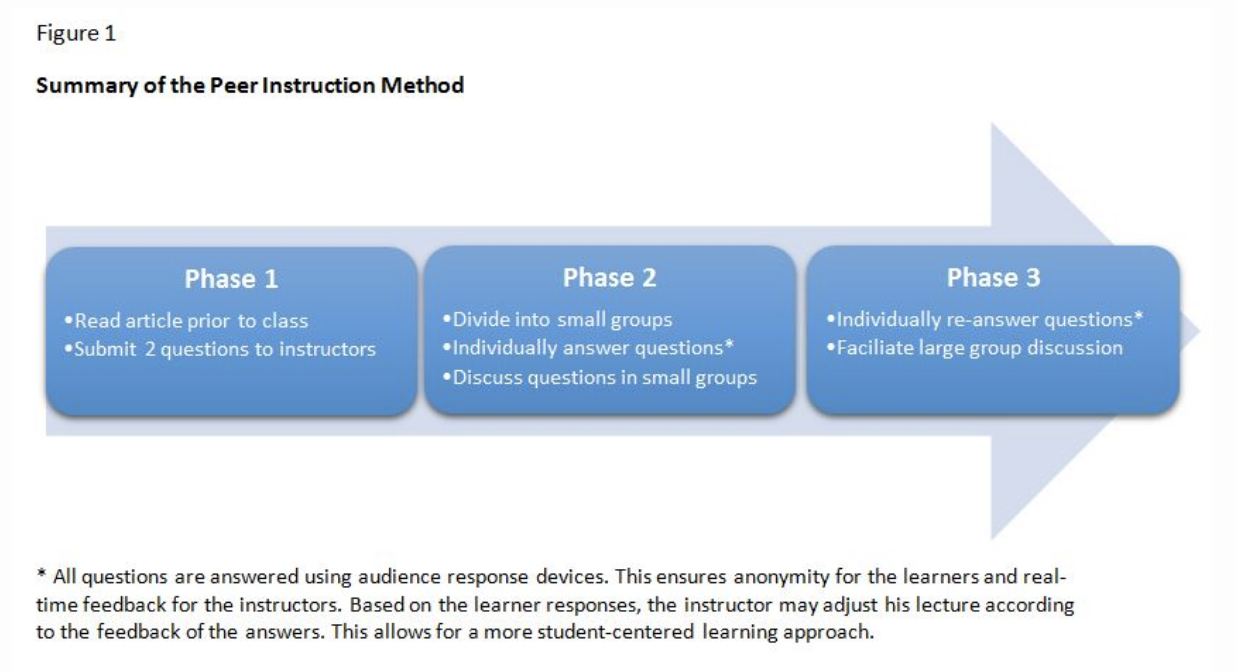
The Peer Instruction Method (PIM) was developed by Harvard Physics Professor Eric Mazur after he realized that physics students were not grasping key concepts during his lectures.2 Mazur invented PIM to facilitate peer to peer learning, which enabled alternative viewpoints that Mazur himself did not consider during his traditional lectures. He found students learn best when they critically think through problems and discuss alternative viewpoints. In this model, students work together to problem solve similar to clinicians on interdisciplinary care teams. Peer instruction accomplishes this by flipping the classroom and creating a student-centered learning environment. A summary of the Peer Instruction Method is shown in Figure 1. This model is flexible, so it may be adapted and modified to different learning scenarios. Because this style of lecture is student-centered, it is imperative that students prepare ahead of time by submitting questions to the instructors.
In an effort to explore innovative teaching methods and provide IPE during didactic sessions, the interdisciplinary instructors decided to test PIM. Prior to our session, formal IPE between pharmacy and medicine was minimal secondary to the distance between the pharmacy and medicine campuses. However, in clinic, pharmacy students routinely work with other medical students and residents to provide patient care. Recruitment of third-year pharmacy students on a 2-week Introductory Pharmacy Practice Experience (IPPE) complemented the medical students and residents already at the practice site. Therefore, the 2-hour session was planned during required didactics for the medical learners and IPPE rotations for the pharmacy learners. The three instructors included one family medicine resident and one physician and one pharmacy faculty member to mirror the target audience.
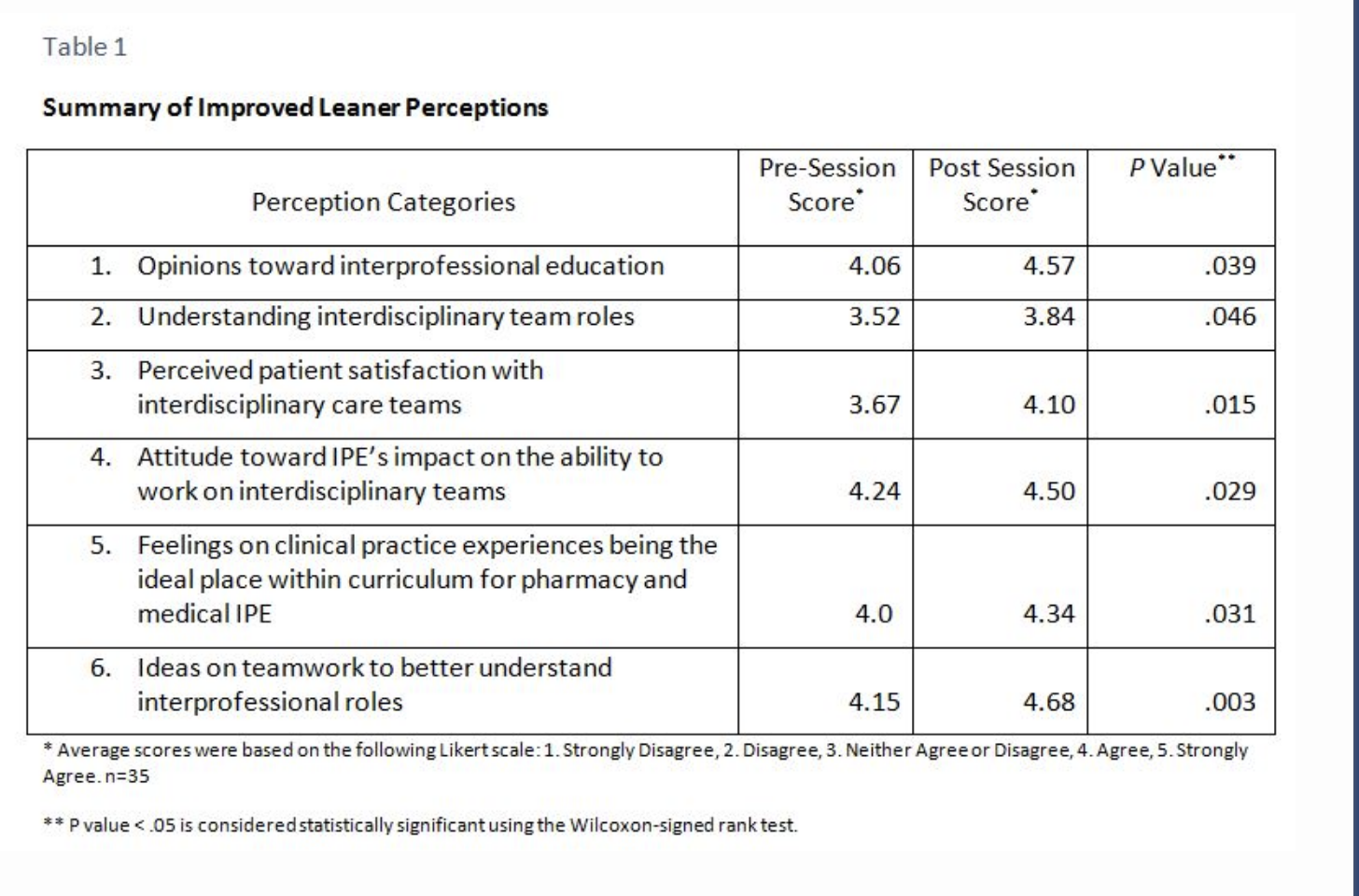
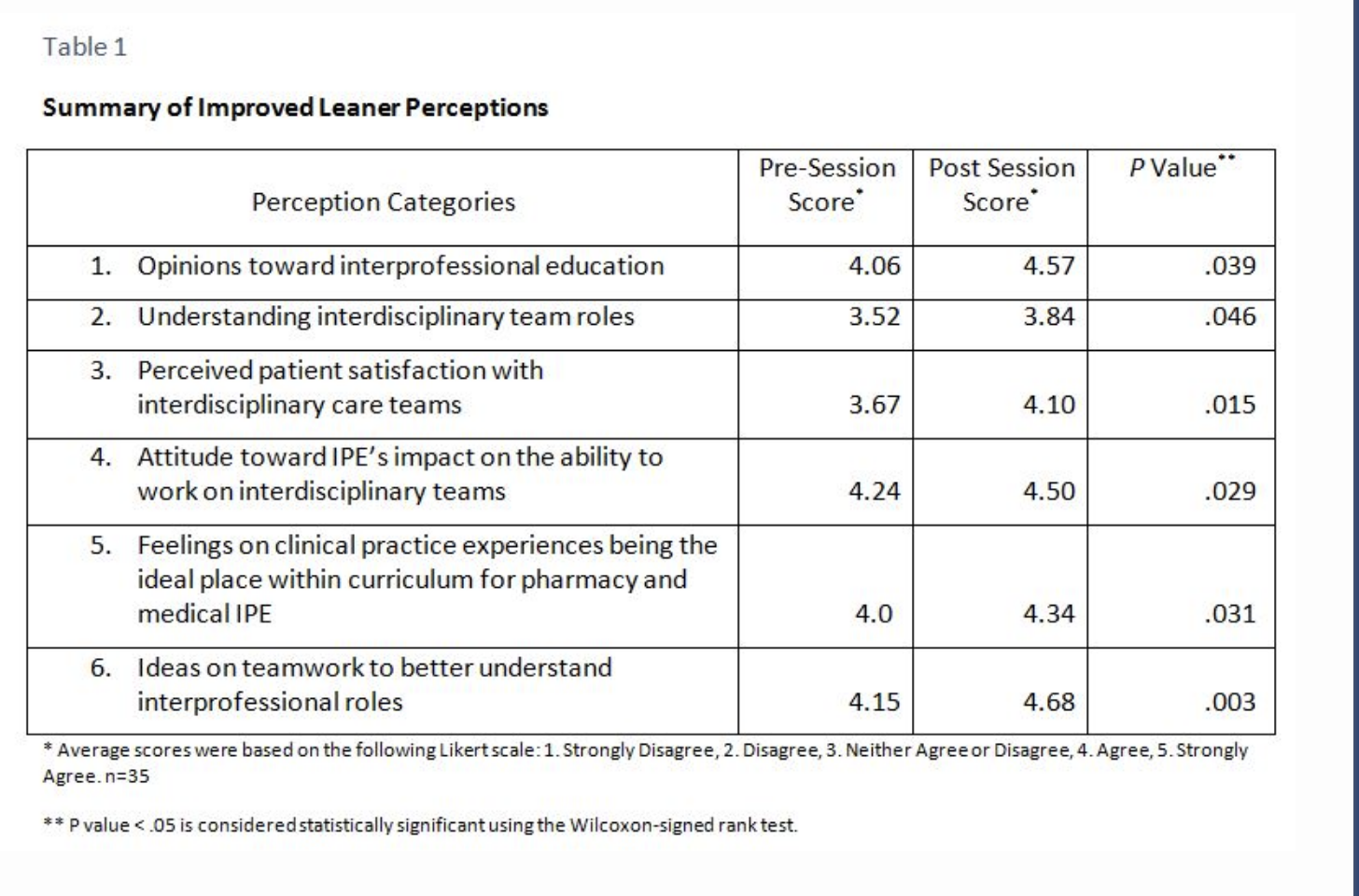
When the learners arrived, every effort was made to evenly distribute them into interdisciplinary teams with five to six members. Instructors planned the 2-hour session based on 80 questions submitted by the 35 learners 2 weeks prior to class, which gave the facilitators the advantage of constructing a session based on learner uncertainty. During the education session, learners were required to answer questions using audience response devices or “clickers” before and after discussion within their group. Facilitators gave adequate time for small groups to discuss their answers and proceed to generate a large classroom dialogue. All participants were given the opportunity to speak, allowing for the expression of viewpoints from the different professions. Each participant was not required to speak, but the instructors tried to gain alternative viewpoints from different groups and professions to facilitate the discussion. A large part of the learning stemmed from the sharing of these viewpoints within the class. A subjective measure of IPE was observed from student responses in class, for example, “Before I thought this . . . but after talking to (other health care trainee), I now feel this is the right answer.” Further, the learners were surveyed before and after the session on attitudes toward IPE providing objective data. Table 1 illustrates six perceptions that improved as a result of the session. Further analysis showed that changes in perceptions were not profession specific but reflective of the learning community as a whole.
Barriers
Scheduling remains a significant problem when facilitating IPE activities, especially when the medical and pharmacy campuses are located 4 hours apart. We recommend planning with pharmacy IPPE students combined with required didactic sessions at family medicine residency programs. This plan allows the combination of pharmacy students, medical students, and residents to participate together.
IPEC recommends IPE occur among students with similar years of experience.3 The family medicine residents in this study have several years more training compared to the other participants and therefore made a clinical topic unrealistic. Instead the session was focused on working with a pharmacist in a patient-centered medical home. We felt this topic would allow open and varying viewpoints during discussions regardless of profession and training.
Conclusions
The Peer Instruction Method is a valuable teaching technique ideally suited for IPE and is consistent with IPEC’s Core Competencies. It can be integrated into family medicine residency didactic sessions, but careful scheduling and topic selection are critical. The development of a student-centered learning environment focused on sharing alternative viewpoints to answer questions among interprofessional groups is accomplished with the PIM.
References
- Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice: Report of an Expert Panel. Washington, DC: Interprofessional Education Collaborative, 2011.
- Crouch C, Mazur E. Peer instruction: ten years of experience and results. Am J Phys 2001;69(9):970-7.
- Buring S, Bhushan A, Broeseker A, et al. Interprofessional education: definitions, student competencies, and guidelines for implementation. Am J Pharm Educ 2009;73(4):59.