Model of Precepting: Qualitative Analysis of Resident Preferences
Julie Radico, PsyD, MS; Stephanie Gill, MD, MPH; Linda Kanzleiter, DEd, MPsSc, Penn State Milton S. Hershey Medical Center
Teaching is a complex process in residency education. Unspoken expectations can be challenges to maximizing learning outcomes. Residents and faculty preceptors may have different ideas as to how residents learn best. If learners and teachers approach precepting with different styles for learning in mind, both parties may walk away unfulfilled. Similar mismatches have been found between patients and physicians in their explanatory models of illness.1 We completed a pilot study to determine if there is a difference between what residents believe best facilitates their learning and how preceptors teach and believe residents want to learn.
Residents and precepting faculty from the Family and Community Medicine Department at Penn State Health Milton S. Hershey Medical Center and State College were asked to participate in this IRB-approved research. Residents and faculty were recruited to take part in focus groups regarding faculty precepting. Four focus groups were completed—two PGY-1 groups totaling ten residents and two faculty groups totaling ten preceptors. The focus groups were conducted by Dr Kanzleiter. Questions included:
- What makes a good outpatient preceptor
- What makes a good inpatient preceptor
- What makes a preceptor’s teaching stick and lead to learning?
- What do you value in precepting?
- What motivates you during precepting?
- What do you expect from good precepting?
- What makes learning during precepting different than learning a hobby?
Qualitative analysis was completed through grounded theory. It resulted in five themes of what residents and preceptors value, are motivated by, and expect related to learning through precepting. These were: time, specific strategies, responsibility, preceptor needing to attend to the resident, and resident autonomy.
Time
Residents’ time in training and the time of year were reported by residents and preceptors to impact precepting. Preceptors said their teaching strategies changed depending on where the resident was in their first year. Residents reported feeling they should receive more guidance earlier in the year and less later. Preceptors did not state specific changes in the intensity of their guidance throughout the year. However, they spoke about changing what they focused on during precepting based on resident time in training.
Residents reported the length of precepting and the wait time to precept hindered their interest in learning. Residents endorsed that lengthy precepting caused them to stop learning and strategize on which preceptors to pick in the future.
Specific Strategies
Importance was placed on preceptors sharing specific strategies (eg, decision making and increasing efficiency). One of the strategies emphasized was having the residents learn by doing. For example, having them complete a procedure or use a risk calculator.
Responsibility
The importance of providing the best care and avoiding harm was expressed. Residents were comforted in knowing they had a preceptor helping them ensure patients get the best care. But, they were also aware that they needed to learn to avoid mistakes “because what if nobody catches it?”
Preceptor Needs to Attend to Resident
It was clearly expressed that preceptors have many demands on their attention. However, both residents and preceptors felt it was imperative that residents receive undivided attention for the best learning to occur. A preceptor could provide this attention by not looking at their laptop, making eye contact, and not responding to other demands (eg, staff members’ questions) during active precepting.
Autonomy of Resident
It was important for preceptors to not take over the appointment when seeing the patient during precepting. For example, residents said they want to use their preferred plan, if it is an appropriate plan, even if it is not one the preceptor would have chosen. Also, residents said they want the message to the patient to come directly from them, not from the attending. This way, the patient is looking at the resident and identifies them as their primary care physician.
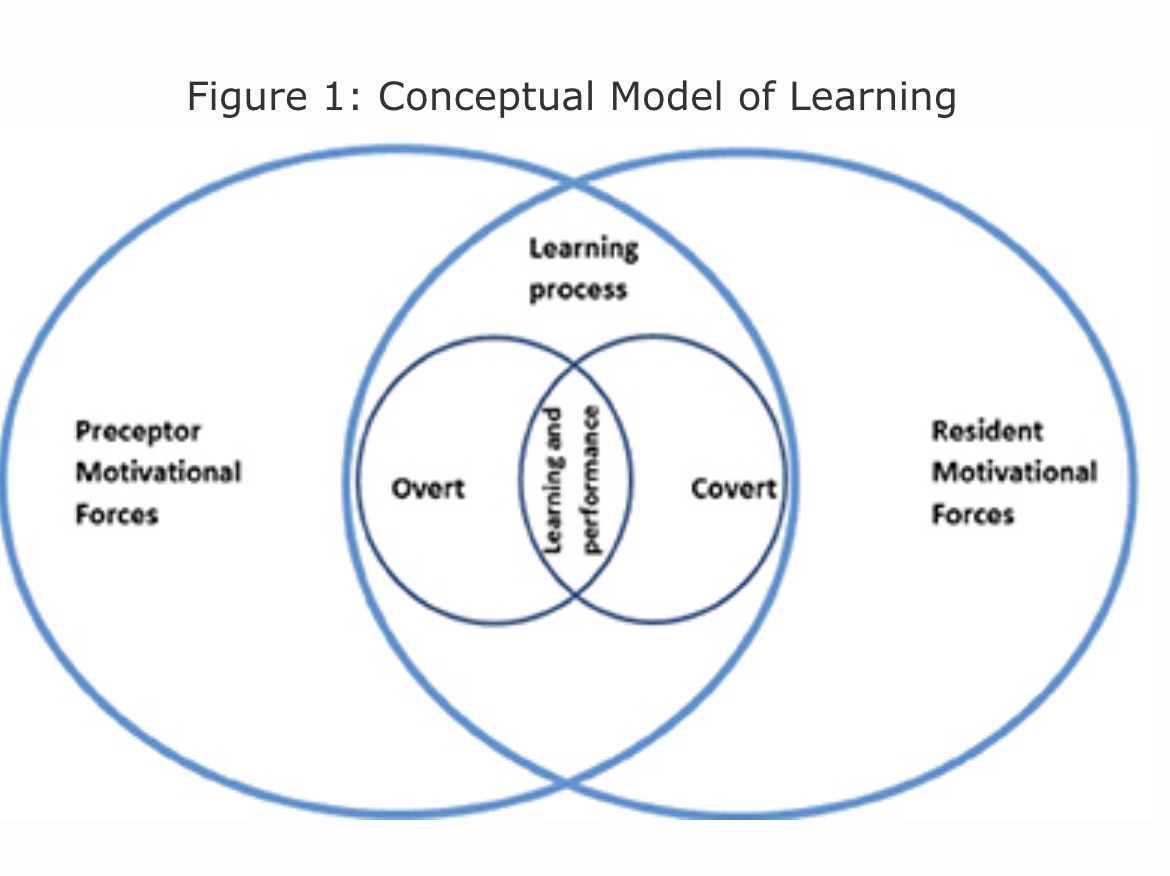
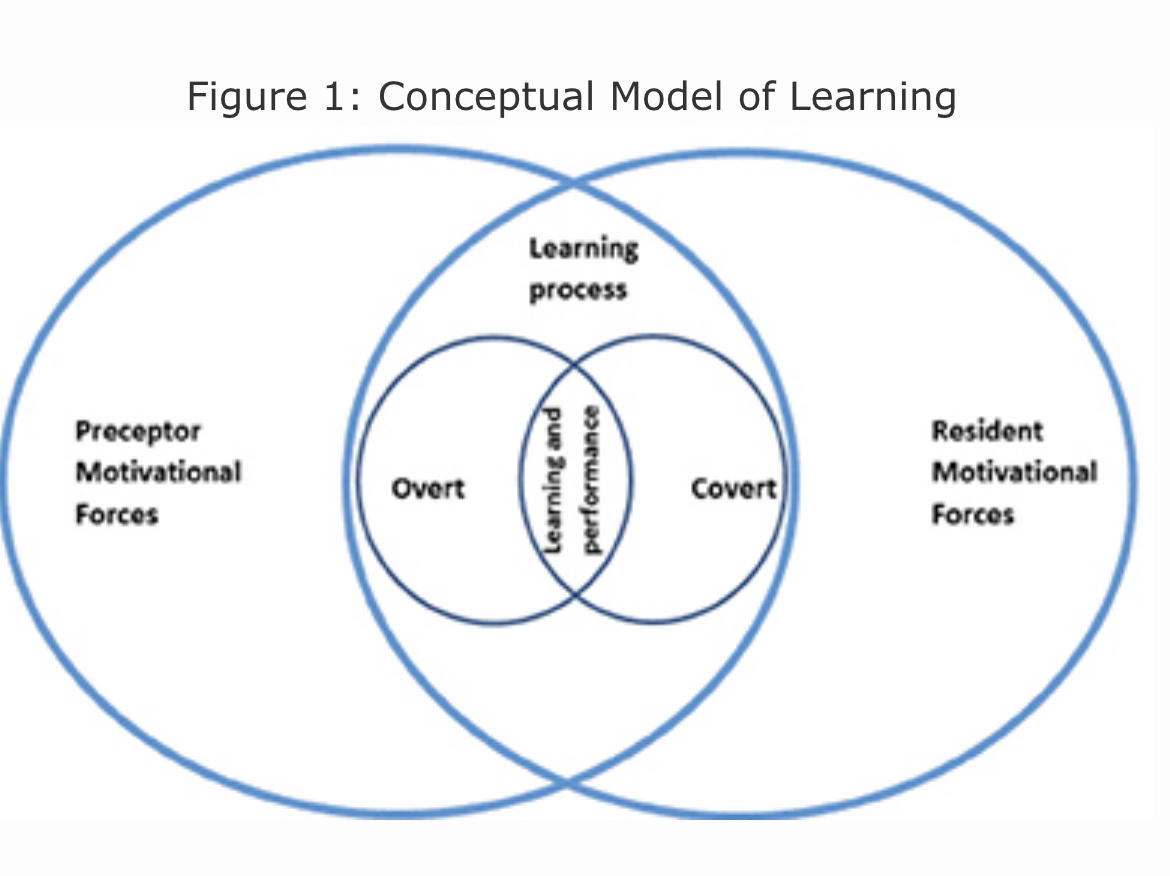
Conceptual Model of Learning
We further grouped these themes by covert and overt motivational forces to generate a model of learning (Figure 1). This model recognizes the impact of these forces brought by residents and faculty to precepting, which in turn influences learning and performance. Covert forces are motivations not readily shared aloud. For instance, residents reported wanting to complete precepting quickly, resulting in them being strategic in their choice of preceptor. Residents reported preferring a preceptor who was quick and one who knows the patient’s background already. Additionally, residents reported already knowing what they wanted to learn from the preceptor for a patient encounter. They did not attend as much to precepting after that information was gathered. Overt forces include stated factors that impact learning. For example, a resident might state they have two patients waiting and ask that precepting finish quickly. It is important for both residents and preceptors to utilize strategies to better communicate needs during precepting and check in with each other to make sure the receiver is getting the intended message.
References
- Street RL Jr, Haidet P. How well do doctors know their patients? Factors affecting physician understanding of patients’ health beliefs. J Gen Intern Med. 2011;26(1):21-27.
https://doi.org/10.1007/s11606-010-1453-3.